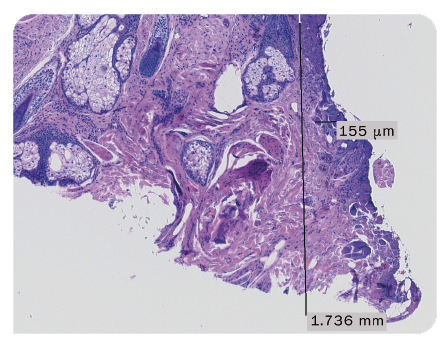
Fig. 1: Lateral thermal damage following radiofrequency excision: 155 µm*
Fast wound healing and good cosmetic results are of great importance in skin surgery. The CURIS 4 MHz radiofrequency technology enables precise cutting with minimal lateral thermal damage1,2, offering a suitable solution for a variety of applications in dermatologic surgery and plastic & aesthetic surgery.
Dermatologist R. Kasten, MD, from Germany reports about his experiences with the CURIS 4 MHz radiofrequency generator in his practice:
“Radiofrequency surgery causes less lateral tissue damage than conventional electrosurgery. Consequently faster wound healing and a better cosmetic outcome can be expected. Studies have even shown better cosmetic results for radiofrequency skin surgery than for CO2 laser applications. Radiofrequency also improves operation comfort by enabling pressure-free cuts with minimal bleeding in a very cost-effective way.“
R. Kasten, MD, Mainz (Germany)
As seen in the histological assessment (Fig. 1 and 2) the application of the 4 MHz radiofrequency technology produces less lateral thermal damage than conventional highfrequency technology.
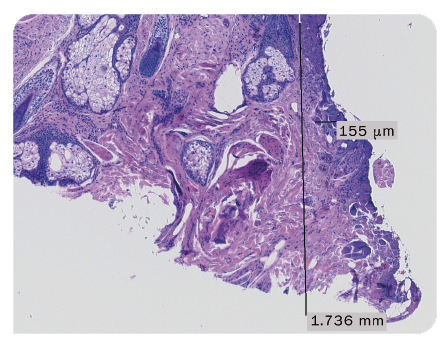
Fig. 1: Lateral thermal damage following radiofrequency excision: 155 µm*
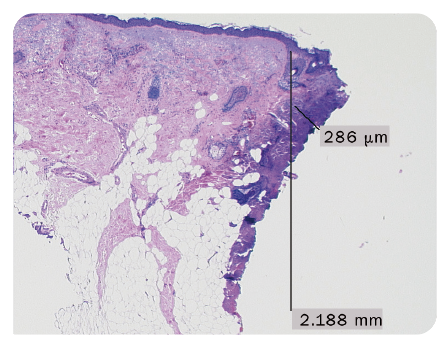
Fig. 2: Lateral thermal damage after conventional electrosurgery excision: 286 µm*
* courtesy of Dr. Kasten, Mainz (Germany)
Find out more about the study results by R. Kasten, MD, in the application report:

The ARROWtip monopolar microdissection electrodes, single-use, provide a suitable precision instrument for the application of the 4 MHz radiofrequency technology in dermatologic surgery. With their heat-resistant and ultra-sharp tips, they enable precision for fine skin and tissue incisions and coagulation. Sutter offers a selection of different models adapted to different needs in the OR.
Find further opinions by surgeons and an overview of the wide range of solutions with the CURIS 4 MHz radiofrequency generator in the catalog Dermatosurgery and Plastic Aesthetic Surgery.
References:
1 Hoffmann TK et al. Comparative analysis of resection tools suited for transoral robot-assisted surgery. European Archives Oto-Rhino-Laryngology. 2014; 271 (5) : 1207-1213
2 Hofauer B et al. Radiofrequency in Oral and oropharyngeal tumor surgery. Auris Nasur Larynx, 2020; 47(1):148-153.